On March 1 Pennsylvania announced the further loosening of many COVID restrictions, including eliminating the requirement to quarantine if traveling from out of state. It should be noted that this is still not a complete rescinding of all restrictions and OF COURSE everyone should still be wearing masks, distancing, washing hands, and avoiding (unmasked) indoor gatherings. In fact, given the context of dropping, but still high transmission rates, still quite limited vaccine coverage, and increasing threat of easily transmissible variants, we should be looking ahead with a mix of both optimism and caution and doing what we can to ensure the best outcome possible.
Even though travelers are now no longer required to test or quarantine upon arrival or return to the state, you could still find yourself in a position of needing to minimize risk of exposure and choose to do so on your own. It is still a good idea to think through the logic of the process and understand the timelines involved. For example, someone I know is planning on going to help his daughter post-op in another state. Both households are working through the timing and figuring out how to limit exposure for all concerned. For another example see below for an extended discussion of what has been playing out at many colleges where a large number of people traveled back to campus all at once not so long ago (hint: those are circumstances under which a careful quarantine really ought to be observed, though in many cases it wasn't).
As ever, it is hard to know exactly what is going on from day to day and February proved to be a poster child for uncertainty. We got lots of test results reported, but don't know when they were administered. We got a lot of university student cases reported, but they were posted to public tallies out of sync with their appearance on campus. We started gearing up to get vaccinated, but ran into roadblocks with limited supply which rendered an already confusing process extraordinarily frustrating.
The reality is that for some subset of those skipping the thoughtful part of the process, there will eventually be occasion to work through it all in reverse in the form of contact tracing, reviewing who you might have exposed during the interval in which it turns out you were infected but as yet unaware of it. That also just brings home how we can/should all still be considering ourselves as potential vectors and continue to take steps to minimize whatever risk we might present to others -- masks, distancing, hygiene, and avoiding indoor (unmasked) gathering STILL for the win.
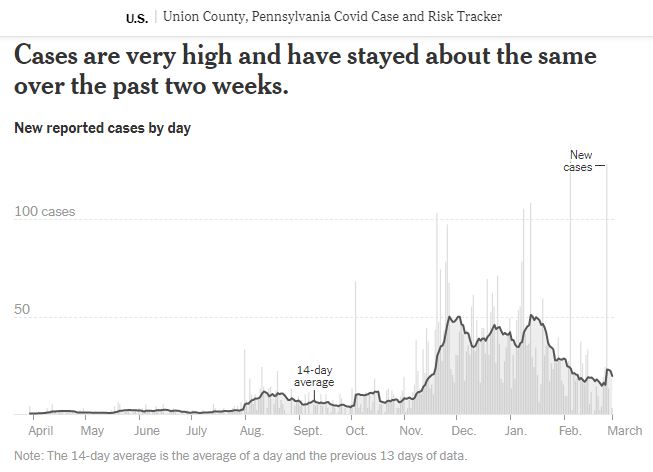
We we can look at our stats right now and feel concern but also modulate that concern with understanding that instantaneous numbers are the least precise thing we can focus on and that the trend over the past two months was for an overall general and significant rise in cases and then an ensuing drop, with the return of students to the area complicating that trend. The real question will be whether any of the variants have made their way here in the interim and who will win in the "infections v injections" race.
The below essay was published in the Williamsport Sun-Gazette on Saturday, February 27, as part of a collaboration on regional public health messaging with the Lycoming-based Let’s End COVID group:
What is happening with COVID-19 cases at area colleges and universities, like Lycoming College and Bucknell?
Many colleges and universities around the country delayed the start of the second semester, seeking to avoid the expected surge in cases over the holidays. By now, though, those who are returning in person have done so. And it has proven challenging even on the far side of the national winter peak. Whereas in much of the country case levels remained moderate until right before Thanksgiving, most areas are now at infection levels similar to those from early November when most campuses closed. Numbers are dropping, but it is a much more fraught context in terms of potential exposure than September.
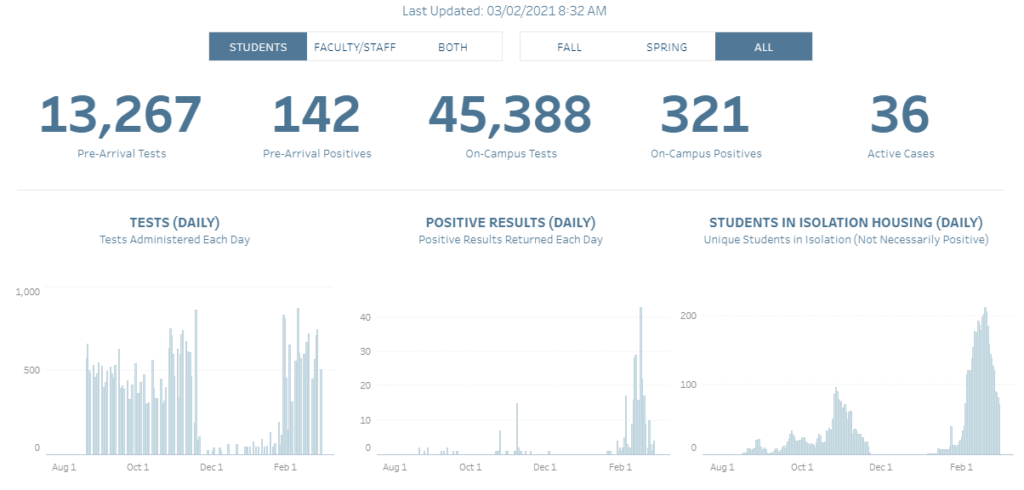
Students on many campuses in the fall were undergoing assurance or surveillance testing, meaning that they were screened for infection at regular intervals regardless of exposure or symptoms. That helped schools keep tabs on cases that would otherwise have gone undetected, given the tendency for minimal symptoms in that age group. When the students went home over winter break, though, that testing stopped. Student exposure changed but was not eliminated, so cases would have continued.
Most schools did require students to get tested before or upon return for this semester – and even more importantly they started or resumed assurance testing. While the entire country was experiencing the winter surge, there were likely also many cases (even if not a surge per se) in the college age population, just undetected. That cohort has brought some of those under-the-radar cases back with them to campus. Luckily they are being identified, largely thanks to assurance testing.
Why didn’t having students provide negative tests to start with catch all the cases?
That comes down to the limitations of testing, which are frequently misunderstood and ignored. Many people imagine that if they’ve had a negative COVID test, they have a clean bill of health; some even mistake it for a license to behave less carefully.
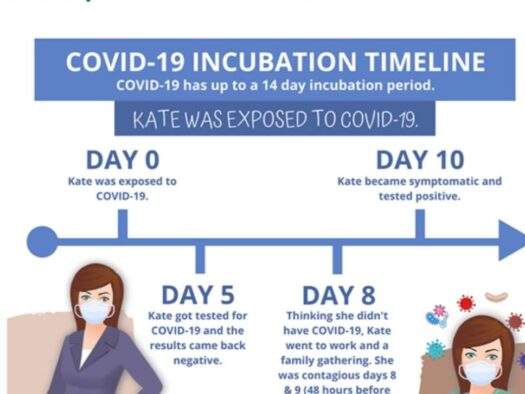
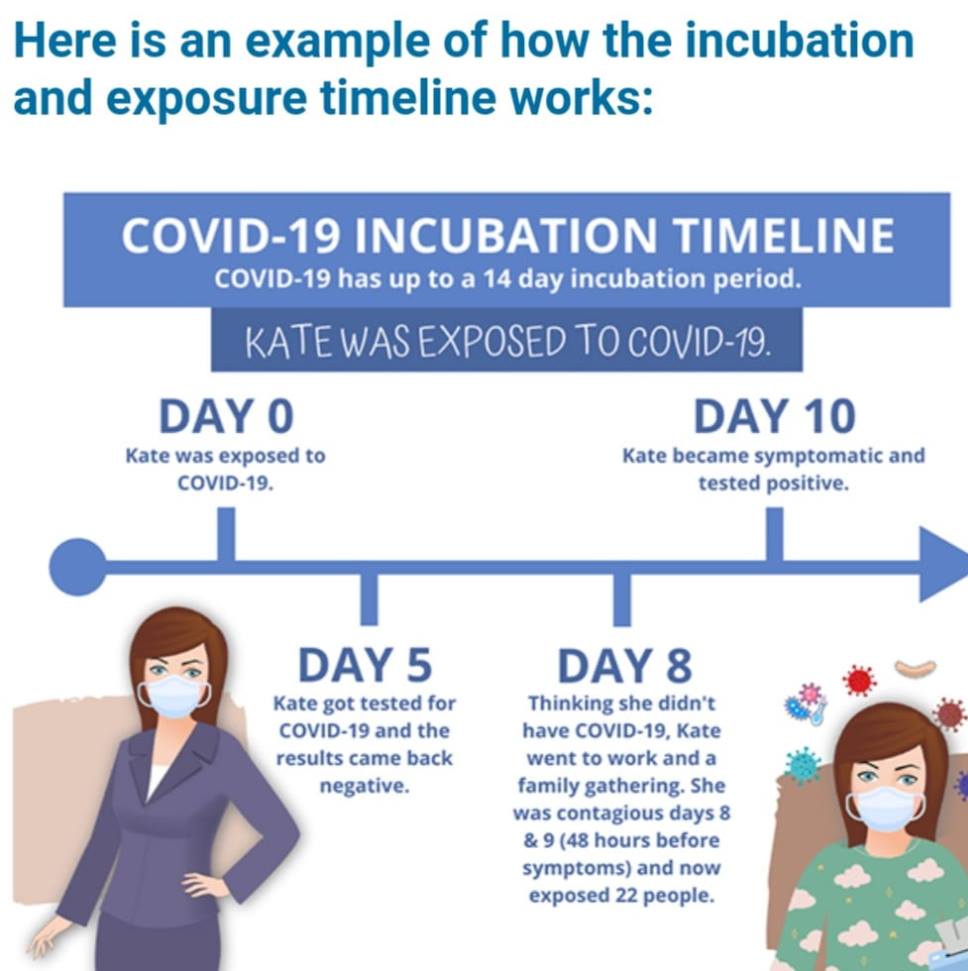
It seems straightforward: a negative test says you don’t have COVID, right? Well, there are caveats. It really says you probably didn’t have COVID at the time of the test – though it might be wrong, false negatives are not uncommon -- and it doesn’t say anything at all about how you have fared since. In fact, a test can’t identify an infection you harbored at the time if it was still incubating. You could test negative, possibly several times at short intervals, and later go on to develop a case based on an exposure that happened before the tests – not to mention subsequently!
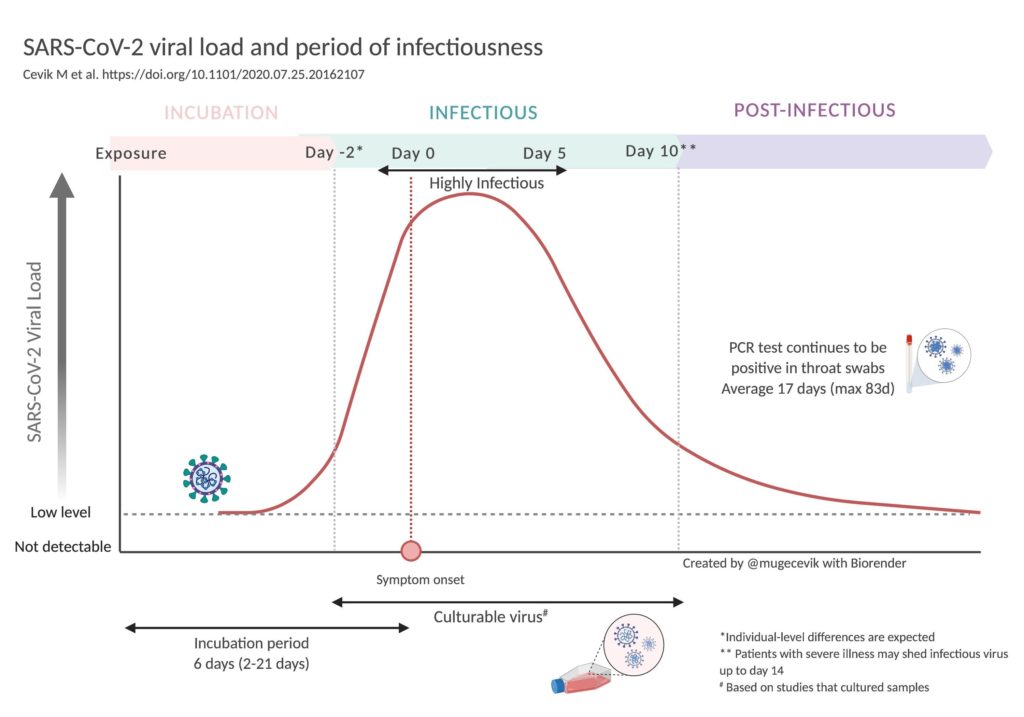
Take this timeline for example: You’re a college student who lives with your family. Unbeknownst to anyone, someone in your household picks up an asymptomatic case and becomes infectious about a week before classes resume, say on Sunday, January 24. So you get exposed that day. The virus enters your system, but is incubating. You dutifully go and get tested. At that point, you are still incubating and not yet detectable (also not yet infectious). By Sunday, January 31, you are on campus with your negative test results -- even multiple negatives -- in hand, but also possibly either already infectious or about to become so some time in the next week. Perhaps you interpret your negative tests as indicating that you are “safe,” and you let down your guard upon seeing your friends again. Or maybe you are careful but you still unintentionally expose people you share living quarters with…
It’s easy to see how this can go wrong. The 2 to 14 day incubation period can really trip us up when it comes to understanding test results -- especially in combination with being infectious before and/or without symptoms.
But if that is the case, then what is the point of all the testing?
It is admittedly less useful on an individual basis, but on average it will help to identify more cases, especially pre-symptomatic and asymptomatic ones that would otherwise be easily missed. What’s more, combining testing with careful quarantine helps make the test results much more reliable. If, for the two weeks before returning to school, you isolated from your family members, wearing masks when together and taking meals apart, you could have more confidence that a negative test was indicative of a clean bill of health and that there wouldn’t be an infection lurking/incubating in your system. Once back on campus, of course, you would want to maintain your caution and vigilance with masks, distancing, hygiene, and avoiding indoor gathering, recognizing everyone else as potential infection incubators, too.
It’s complicated to juggle the logistics of quarantine and the logic of testing. It can seem unreasonable and too confusing, but as an alternative to locking down entire campuses after outbreaks, such precautions look more manageable in retrospect.
Every bit helps – so keep wearing those masks, too!